
Scott Matzka first noticed something was wrong when his finger locked up while applying drywall at home in Kalamazoo.
The retired University of Michigan and pro hockey player soon developed other troubles: a hand that refused to unclench, a forearm that cramped suddenly. Eventually Matzka was diagnosed, at 36, with limb-onset amyotrophic lateral sclerosis, or ALS — also known as Lou Gehrig's disease. ALS is a neurodegenerative disease that can manifest in many ways, but which bodes a short lifespan.
"There is really nothing that you do after [diagnosis] except try to go live your life," Matzka says.
But a door onto the ALS mystery is opening, raising hopes for a future with effective therapies for patients like Matzka. New research shows that seemingly unrelated conditions like ALS, heart disease, diabetes and aging have something in common: misfolded proteins in the cell.
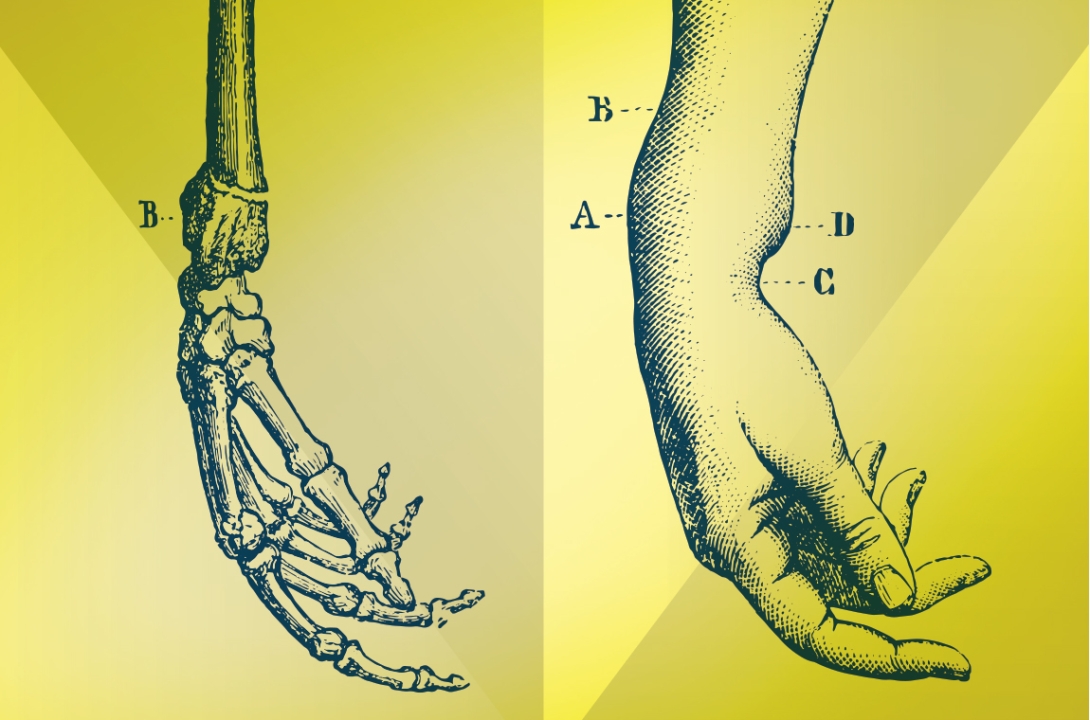
Proteins are long strings of amino acids that must twist, double up and fold in on themselves, morphing into just the right shape to assume their proper place in the cell's machinery. The cell has several complex "quality-control" processes to help ensure this goes smoothly and that faulty proteins are repaired or removed. Many diseases in different organ systems have been found to occur in part because protein folding has gone wrong.
U-M researchers are now studying those folding flaws in a cross-disciplinary research effort called the Protein Folding Diseases Initiative, or PFDI. Some 70 researchers from around the university are exploring the basic mechanisms and consequences of misfolded proteins in human diseases like ALS. This approach holds promise because it may lead to new drugs, or repurpose existing ones, in order to help patients who might be running out of options.
The Need to Cross Disciplines
Protein misfolding is at the heart of many neurodegenerative diseases like ALS, but it happens in cardiac, endocrine and other organ system diseases as well. Any fundamental discoveries about the process could lead to breakthroughs in various medical specialties. So the initiative brings multiple forms of expertise to bear on basic questions, like: How do proteins misfold and why can that lead to disease?
"In some cases, the diseases are so complicated we just don't know enough," says PFDI scientist Geoffrey Murphy, Ph.D., associate professor of molecular and integrative physiology, whose lab studies memory and aging. "We really need to understand the basic biology, so we can have some understanding of how it all works normally and how it all works when it's abnormal. That's where the Protein Folding Disease Initiative really captures it."
The initiative is not a discrete place, but a network of collaborators across campus. They have organized into four hubs, each of which holds meetings to discuss early research ideas; researchers in different hubs also mix at monthly seminars. Annual gatherings help get the word out and attract new researchers.
In fact, many initiative researchers say that its greatest asset is in its ability to connect scientists who are passionate about similar areas of science, but who might not otherwise meet across academic or physical boundaries. At present, its members hail not only from the Medical School but also from the Life Sciences Institute; the College of Literature, Science, and the Arts; and the College of Pharmacy. All of them enjoy reduced-cost access to powerful resources like a brain bank and a reagent library.
Such access "reduces the potential barriers to looking at questions beyond your discipline," says Henry Paulson, M.D., Ph.D., one of two researchers who co-directs the initiative.
He hopes to recruit new scientists from outside the fields currently represented.
"Tackling a human disease doesn't just require medical school personnel," says Paulson, who is the Lucile Groff Professor of Neurology and director of the Michigan Alzheimer's Disease Center. "People from basic science, chemistry, pharmacy, the School of Public Health, engineering — we need those connections to really have maximum impact."
In fact, some non-PFDI-affiliated groups on campus may already be studying protein-folding diseases, says Peter Arvan, M.D., Ph.D., chief of the Division of Metabolism, Endocrinology and Diabetes. They just may not be treating protein folding as the crux of the problem.
"In a lot of cases, the doctors or the scientists who are working on these diseases are worrying about how to replace the loss of function [when] there's a certain protein whose function is missing. … That's one approach," Arvan says. "The protein-folding diseases approach is actually to work on the misfolded proteins themselves — either to fix or degrade them, or to find chaperones to help them or replace them."
While its emphasis is on fundamental understanding, the initiative also has a translational arm. Working with the Center for the Discovery of New Medicines, or CDNM, several PFDI scientists doing drug-discovery projects met this fall after the symposium with pharmaceutical industry representatives, including Pfizer and Abbott.
Vince Groppi, the CDNM's director, calls it a way to "pressure-test" the projects, giving investigators immediate feedback about what their project might need to accomplish before partnering with industry to bring a new drug through to the clinic. "Early input helps us move projects to the clinic faster by identifying problems early on," Groppi says.
The PFDI began five years ago when researchers at the Medical School were asked by then-Medical School Dean James O. Woolliscroft, M.D., to envision new cross-disciplinary, centrally-funded research programs. Paulson and Andrew Lieberman M.D., Ph.D., the Abrams Collegiate Professor of Pathology, came up with a protein-folding disease proposal. Of 10 proposals, it was one of two chosen, and received $9.3 million.
In turn, the initiative has garnered some $28 million in new grant money since its inception, allowing it to fund new projects within the university. Paulson also credits it with helping the University of Michigan secure National Institutes of Health funding for the Michigan Alzheimer's Disease Center, among other projects and centers. In hopes of translating results to the clinic as soon as possible, some researchers are also connecting with pharmaceutical experts about promising leads.
To Matzka, resources that go well beyond what activists can raise — like the Ice Bucket Challenge — is a key source of hope.
"When we get the government and Big Pharma to pay attention, I think that we have a chance," Matzka says.
While ALS is relatively uncommon, he adds, the closely related Parkinson's and Alzheimer's diseases are very common. Six million people in the U.S. are living with one or more of these conditions.
"To me that paints a different picture — not of it being some rare, obscure disease, but maybe being more of a neurological epidemic," Matzka says. "I'm sure that by finding something that helps ALS, it will in turn help Alzheimer's and help Parkinson's."
The Science of Misfolding
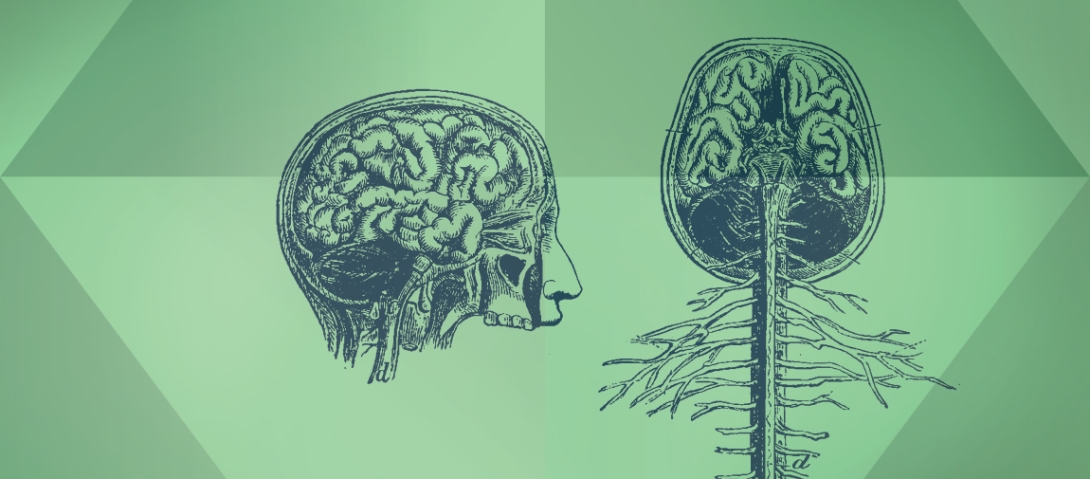
That's not an unwarranted assumption. Misfolded proteins are at the heart of many neurodegenerative diseases. Ataxias, Parkinson's disease, and Alzheimer's disease all have protein folding problems in common.
For instance, Matzka's physician, Eva Feldman (Ph.D. 1979, M.D. 1983, Fellowship 1988) studies a protein whose misfolding has been noted not only in ALS but also in a related neurodegenerative disease called frontotemporal dementia. When this protein misfolds in neurons, it often accumulates, causing neuronal death. Its release from dying cells can also damage neighboring neurons. This might help explain the oddly nonlinear way that ALS progresses: it can start in one limb, then jump to a different place in the body.
Feldman and other initiative researchers studying ALS, including assistant neurology professor Sami Barmada, M.D., Ph.D., and cell and developmental biology professor Lois Weisman, Ph.D., whose lab is at the Life Sciences Institute, are cautiously optimistic about the potential for insights about protein folding to lead to new therapies for ALS.
One possible strategy lies in stimulating one of the cell's natural defenses against misfolding. Called autophagy, or "self-eating," it's how a cell dismantles broken and unnecessary molecules. Stimulating autophagy in ALS cells that have a misfolded protein can dramatically improve outcomes, Barmada says. He and Weisman used those results to secure a pilot grant through the initiative, which they are using to create new cell lines to study autophagy.
MISFOLDED proteins are at the heart of many neurodegenerative diseases. Ataxias, Parkinson's disease and Alzheimer's disease all have protein folding problems in common.
Other drugs seem to intervene in faulty folding processes as well. A drug screen by Maria do Carmo Costa, Ph.D., a researcher in Paulson's lab, found that the common antipsychotic drug aripiprazole handily reduces levels of a toxic protein in models of a disease called spinocerebellar ataxia type 3. Funded through a PFDI pilot grant and the Center for the Discovery of New Medicines, the study appears in the November 2016 issue of Brain.
Murphy, the memory researcher, studies the connection between metabolism and Alzheimer's. His group has preliminary data suggesting that an antidiabetic drug called acarbose seems to help mice with a form of early-onset Alzheimer's, a disease that can arise from mutated and faultily folded brain proteins. The drug may also slow the aging process.
Lieberman, PFDI's co-director, has uncovered a drug that stops expression of the protein whose gene is mutated in an untreatable degenerative condition called Kennedy's disease. The mutation causes the protein to unfold, leading to brainstem and spinal cord neuron loss and progressive weakness in affected young men. Plans are afoot for a clinical trial of this drug in the next year.
Misfolding Elsewhere in the Body
Neuroscience isn't the only area where initiative researchers are exploring the link between protein folding and disease.
Sharlene Day, M.D., is an associate professor of internal medicine and a clinical cardiologist. She studies hypertrophic cardiomyopathy, a heart disease that affects over one in 500 people worldwide. One potential culprit protein in this disease is sometimes mutated in such a way that it gets truncated, misfolds and accumulates harmfully in heart cells. Day's group, through their research into so-called molecular chaperones — a class of proteins that aid protein folding — has found a small molecule called YM1 that speeds up the breakdown of the mutant protein.
In endocrinology, too, protein misfolding can play an important role. Endocrine diseases like diabetes and congenital hypothyroidism can arise from any of dozens of genetic mutations, and many of those mutations lead to the same outcome: the mutant protein misfolds, becomes stuck in the cell's machinery and fails to be secreted. As with cardiomyopathy, this trapping of proteins gums up the works, damaging the cell's function. This is sometimes called a "gain of toxic function" mutation. Cells do have natural defenses against the occasional misfolded protein, but they can become overwhelmed.
"These cells are making hundreds of thousands of molecules of the same protein per minute," Arvan says. "So if a significant fraction of these copies each minute will misfold, the cell is going to have a devil of a time catching all of these bad molecules."
Problems like this can sometimes show up very early in life. In a type of diabetes called mutant INS-gene-induced diabetes of youth, a mutated insulin precursor protein builds up and destroys the beta cells of the pancreas. The result can show up as full-blown diabetes at the age of 10 weeks.
Last year, a New Zealand man whose baby suffers from that form of diabetes flew to Michigan to take part in a video presentation shown at the initiative's October symposium. An emphasis on patient stories and clinical applications was a theme of the 2016 symposium.
Matzka, his motor coordination and voice eroded by ALS, isn't waiting either. He has become an activist, founding an organization called My Turn that seeks to give voice to sufferers of the disease. Though he doesn't closely follow research, preferring to leave that to his physicians, he says the PFDI is "an important part of the puzzle. … It is at least a piece — or several pieces — that we haven't had before now."





