Michigan Medicine responds to social unrest in the midst of COVID-19.
Author |

When Allecia Wilson (M.D. 2004, Residency 2007) saw the video of Minneapolis police officer Derek Chauvin with his knee on George Floyd's neck, she knew what she was witnessing. Like many Americans, Wilson "was struck by the inhumane treatment Mr. Floyd experienced, and blatant disregard for his life," she said at a June 5 virtual protest hosted by the Black Medical Association (BMA) at Michigan Medicine. But as an assistant professor of pathology at the Medical School and director of autopsy and forensic services, she witnessed something else as well. "In my training in forensic pathology, I immediately understood the potential mechanism involved in his death," she said. "I had faith in our medical system and knew the steps and guidelines that needed to be followed. When the preliminary findings were released, I was sure it was a mistake." The Hennepin County Medical Examiner's office classified Floyd's death as a homicide, but listed "cardiopulmonary arrest while being restrained by law enforcement officer(s)" as the cause of death, rather than traumatic asphyxia. In other words, there was room for doubt as to whether Chauvin was entirely responsible for Floyd's death; the report suggested Floyd's underlying health problems may have played a role.
When Floyd's family requested a second autopsy, Wilson was one of two pathologists who took on the work. "I felt that my life experience, my training, and everything I stood for were prepared for this moment," she told the virtual protesters via Zoom. But it wasn't easy. The National Association of Medical Examiners (NAME) published a statement insinuating that pathologists conducting second or private autopsies "have an incentive to come up with a certain view." Incensed, Wilson sent NAME a letter in defense of her work and of second opinions in general, which, as she pointed out, are common in most medical disciplines. NAME has since removed the statement from its website. Wilson says she received an apology from the organization via email, but she is hoping the organization will post the apology online.
As Floyd's death sparked protests across the nation against police brutality and systemic racism, Wilson worked alongside high-profile forensic pathologist Michael Baden, M.D., to complete a second autopsy. Wilson and Baden concluded that Floyd had died as the direct result of the pressure placed on his body by all three of the police officers at the scene. Wilson was quoted in Newsweek: "Second autopsies do have their limitations as we are not seeing the tissues in their original state, but with that acknowledgment, we feel those items will not change or alter the primary cause of death was mechanical asphyxia."
Wilson's autopsy of George Floyd was one of the many responses by members of the Michigan Medicine community and the broader U-M community. On May 29, four days after Floyd's death, Robert M. Sellers, Ph.D., chief diversity officer at U-M, published a personal reflection about his weariness with racism in the U.S. His message reached more than 100,000 people on social media and garnered praise from people across the country.
"This morning, I woke up very tired," he writes. "Not your normal tired. I woke up with a kind of tired that can only be found on the other side of loss, anger, frustration, sadness, and despair. This morning, I woke up in a state in which African Americans make up roughly 13% of the population, but comprise 31% of the people with COVID-19 and 40% of the people dying from COVID-19. I woke up in a country where a White woman can not only accuse an African American man of threatening her because he is simply asking her to obey the law in a public space, but she can actually weaponize the police for her own aims simply by repeatedly referring to him as being African American."
Sellers was referencing the May 25 incident in Central Park, where a white woman, Amy Cooper, threatened to call the cops on a Black man, Christian Cooper (no relation), who was birdwatching and had asked her to put her dog on a leash, per park rules. She said she was going to tell the police that an African American man was threatening her life. Amy Cooper seemed to be relying on a presumption that the police would see Christian Cooper as threatening because of his race and would punish him, regardless of whether he was in the wrong. That is, she understood not only that systemic racism exists, but also that she could weaponize it in her favor.
Sellers' juxtaposition of the Central Park incident with the disproportionate effect of COVID-19 on the Black community underscores the systemic racism inherent in both situations (See "Racial Disparities in the Time of COVID-19"). The protests against systemic racism cannot be separated from the pandemic, which, like Floyd's death, has placed the inherent racism in the U.S. systems of government and health care in stark relief.
Responding in Quarantine
For many at Michigan Medicine, the protests were a call to action to eliminate racism in health care. Faculty, staff, and learners responded with compassion, demands for change, virtual forums, local protests, and personal stories. Approximately 1,400 Michigan Medicine staff and learners took part in BMA's virtual protest, and more than 1,000 people submitted selfies holding protest signs. Their homemade posters listed the names of victims of police brutality: George Floyd, Breonna Taylor, Tony McDade, and many others. Some attendees wrote #WhiteCoatsForBlackLives on their signs, or their profession plus ForBlackLives, such as #NursesForBlackLives and #SocialWorkersForBlackLives.
At the virtual protest, several medical students and physicians spoke about their experiences of racism inside and outside of Michigan Medicine. Here are some of their stories.
Fitz Tavernier Jr. (M.D./MPH 2020), anesthesiology resident

"I was not surprised [by George Floyd's death], not in the slightest. This is nothing new for us. It's something we've been having to deal with for our whole lives. … The first thing that comes to mind is that it could have just as easily been me or someone that I loved. Just because I have whatever degrees or education, that does not make me immune. …
"I grew up in the Grand Rapids suburbs, in a predominantly white neighborhood. In high school I was pulled over with a group of friends. I was the only Black kid, and I was the only one pulled out of the car and placed in the back of the police car. They suspected us of committing a crime, which we were not involved in. The police only called my mother, waking her in the middle of the night to 'see if she knew where I was.' My friends didn't experience anything of the sort. My mom said that the first thing that went through her mind was, 'Something happened to my child.' … She was constantly aware of how people perceive me. That was the first time I understood what it meant to my parents to constantly have to worry about my well-being even in instances where my well-being should not have been compromised."
As an adult, Tavernier was pulled over for speeding. "The first thing out of the police officer's mouth was, 'Whose car is this?' I remember contemplating, 'Why would you try to insinuate that the car I'm driving is stolen? Why couldn't I have just been pulled over as a citizen who was breaking the law … as opposed to reminding me about my race?'
"I constantly have to think about my race. We are consciously always thinking about our race, and many times it's in a way to make sure that other people around us do not feel threatened — not doing it for them, but for our own safety. In an attempt to ensure we don't end up in an unwarranted situation. Shopping at Kroger, in the self-checkout aisle, [I make] sure that all my items are in plain view so I don't get accused of stealing, which I have been, right here in Ann Arbor.
"My very first rotation, I was on OB/GYN. I was accompanying one of my patients to a procedure, and me and my resident were both dressed in scrubs, both had stethoscopes around our necks. I had volunteered to push the patient around the hospital, as she needed wheelchair service. I remember getting in the room and helping the resident set up the space for the procedure. Before the procedure started, I remember the nurse in the room kind of stopped and looked at me and said, 'Do you mind leaving the room? We're about to start the procedure.'
"At first I didn't think anything of it. I was the only male in the room, so I recognized that I could have been making somebody uncomfortable. My resident stepped up and said, 'He's a medical student.' The nurse responded and said, 'I'm sorry. I thought you were a transporter.' Here I am in the same attire as my resident, who's a white female.
"Although [the nurse] didn't have any ill intention, she completely overlooked every aspect of what I was wearing, where I was, what I was doing, and went straight to the color of my skin to … insinuate that I was not capable of being a medical student. I thank that resident who I'll never forget … stepped up, caught the incident, and defended me, and the patient who apologized to me. Afterwards [I thought] … 'this may be a pretty long year.'
"That defines what Black people have to go through in this country. No matter where we are or what we're doing, we are overlooked. The first thing that is seen is the color of our skin."
M4 Stephanie Reyes
"Repeated acts of violence, murder, and targeted hate against the Black community leave a special kind of trauma that you can't shake, that you carry with you in every facet of your life. It started [for me] in college and now medical school and working at the hospital. There isn't a day that goes by that I don't question my value here and I don't question if I'm valued here — if people see me as intelligent enough, charismatic enough, witty enough, special enough … equal to my peers. If I see myself as equal.
"I struggle with internalizing the value that others place on Black lives — people that don't know me, haven't met me — but I somehow succumb to that rhetoric when I feel vulnerable. What I want to tell everyone is that we should all affirm Black lives and do that courageously and ferociously. At the same time, we have to affirm that for ourselves and to think we belong in this space."
M2 Chevaz Thomas

"In the days after George Floyd was murdered, I had a lot of emotions. The first that I felt was anger. I also felt frustration. But in general it was a continuation of paranoia, of fear, of vulnerability, to be someone of color living in this country, to see that after years upon years of Black people getting killed by police, this has continued. It's something that hasn't just started for me with George Floyd dying. I grew up in New York City. I think about the Central Park Five, Sean Bell being killed [by a police officer in 2006]. …
"It made me feel like my skin is a weapon. You feel as though your skin is a threat. You can't really escape it, because the country sees you as a weapon, regardless of your intentions, regardless of what you're trying to pursue for yourself and your family and for … humanity in general, with our career. There's a consistent feeling that you have to soothe other people and make them feel good about your presence in spaces. And that takes a tremendous amount of energy outside of just being a medical student.
"When I get pulled over by police, my first thoughts are, 'What do I need to do to be safe? What do I need to do to make them feel safe … so my mother doesn't get called [and told] that I was dead?'
"While I was on my VA rotation, I had a patient that had cirrhosis, and he came in for a procedure to decrease the pressure in his liver. He had to stay longer after the procedure because he developed more fluid. … His wife came in to calm him down. She says to him, 'I'm not scared of you.' He [says], 'You shouldn't be scared of me. You should be scared of him, the tall Black dude.' In that moment, it just hit me straight on. Even while I'm trying to help other people … my identity is being used against me."
Allecia Wilson (M.D. 2004, Residency 2007), director of autopsy and forensic services

"It was suggested by some, including my national organization, that second, or private, autopsies are done by pathologists who have incentive to arrive at a certain opinion, implying that second autopsies are selling an opinion for money.
"I want to say why I took this case [the second autopsy of George Floyd]. I took the case because I'm a human being with compassion towards others ... because I have an expertise in a very unique field of medicine that focuses on how disease and injury cause death.
"I'm the deceased's final voice. … I get to tell the judge, the jury, and society their final story. I took the case to ensure that George Floyd's story is accurately told, that his voice and the voice of many others are heard."
Michigan Medicine's Town Hall
On the afternoon of June 5, Michigan Medicine hosted a livestreamed town hall to address current events and racism in the health system. "It is extraordinarily sad, indeed heartbreaking, that we are still seeing such terrible acts of discrimination and violence," said Marschall Runge, M.D., Ph.D., dean of the Medical School, executive vice president for medical affairs at U-M, and CEO of Michigan Medicine. "I won't pretend to have any idea what people of color and marginalized people have been going through on a daily basis. … The only way I can raise my cultural awareness, expand my perspective, and deepen my empathy is to listen to the experience of others and to learn from them. As an academic institution, continuous learning and discovery is fundamental to our core. There is no time more demanding than right now for us to lean on this core value." Runge opened the town hall with this call to listen and learn, and most of the meeting consisted of stories about moments of racism inside and outside the institution.
One of the first speakers, a medical student, wished to remain nameless. "This is not about me," she said. "This is about our entire community that's now faced with recognizing and validating the experiences, the identities, and the voices of the marginalized learners, soon to be leaders, right here within Michigan Medicine." The stories she told, collected from other medical students about their experiences of racism at Michigan Medicine, remained anonymous as well, underscoring the ubiquitous experience of microaggression, bias, and racism for Black and brown students.
She told the story of a student who witnessed a fellow telling a racist joke. A nearby attending physician laughed, "almost uncomfortably," and then the conversation moved on. But the student wrestled with whether or not to say something. She felt ashamed when she didn't, but as a "nonwhite woman in a room of only white men," she didn't feel it was safe to speak up. According to a racial climate survey of U-M medical students conducted by the anonymous medical student speaker, 61.5% of respondents never report incidents like these, because of fear of either repercussion or inaction.
Another student was working in a clinic with an attending physician. After seeing an African American patient, the attending said the patient was likely there because they were drug-seeking, "as most Blacks that attending had seen in the past."
In another story, a student was performing a physical exam on a patient, when the patient asked, "Are you going to be able to perform the exam with that thing on your head?" The patient was referring to the student's hijab.
Others at the town hall told their personal stories. Cathy Kendrick, RN, associate chief nursing officer at the Frankel Cardiovascular Center and University Hospital, talked about a recent conversation she had with her 40-year-old African American son. He said, "Mom, I cannot come to your house to help you today [because] I can't figure out a route to get to you anymore. They told us to stay home, stay out of the suburbs, because we are not going to be safe."
Kendrick also talked about the lack of diversity she's seen among her colleagues. "When I can sit in a room for my entire career and I can count the number of people who look like me, that's a problem."
Fourth-year otolaryngology resident Terrence Pleasant, M.D., talked about the pride he felt as a Black student who made it to medical school at Georgetown University. Then "a white woman approaches me on the medical campus and immediately, without hesitation, hands me her keys and instructs me to park her car," he said. "What is it about my attire, my white coat, my bowtie, my freshly pressed shirt and slacks, my stethoscope around my neck? … It had nothing to do with my attire, but … my skin color for her created no ambiguity about the possibilities of what I could achieve in my life."
Later, as an intern in the U-M surgical ICU, Pleasant "was walking down the hall in a group with my non-Black colleagues, again wearing my long white coat, stethoscope, scrubs, and hospital ID badge." A hospital clerk was watching him. When he asked if there was anything he could help her with, she responded, "No, you look suspicious." Pleasant felt "enraged but calm" as he asked her, "Is it because I'm a Black man wearing a white coat?" He says, "My fear was initially limited to 'driving while Black,' … but now I find that even at work, I'm at risk of being seen as a threat."
Dana Habers, chief department administrator of Radiology, and Justin Dimick, M.D., professor of surgery and chair of the Department of Surgery, spoke at the town hall about their experiences of white privilege. Habers said she hopes her three white sons will learn to recognize and give up their privilege, and Dimick spoke about the shame he feels at the privilege of being able to ignore injustices detailed in the news in order to do his work productively.
"We are running out of time."
Erika Newman, M.D. (Residency 2008), associate professor of surgery, spoke at the town hall about the urgency of dismantling racism. She quoted Martin Luther King Jr.'s "Letter from a Birmingham Jail." His words from 1963 about "hate-filled policemen [who] curse, kick, and brutalize, and even kill your Black brothers and sisters" echo the police brutality that sparked protests in 2020.
"Justice too long delayed is justice denied," Newman quoted King. She also spoke in her own words about the need to make immediate changes. "We are running out of time," she said. "We are at a tipping point. We must act now to shift the paradigm of injustice. It is time for drastic change. As doctors and health care providers, we take an oath to treat all patients equally, yet all patients are not equally well." She spoke about the structural violence in the U.S. health care system, where "poverty, poor health, diseases — these all spread along lines of marginalization and race."
Where do we go from here?
At the town hall and in other forums, many at Michigan Medicine requested that the institution commit to antiracism and make significant changes to dismantle the structures of racism in health care. As Feranmi Okanlami (M.D. 2011) said at a June 4 webinar organized by the Department of Urology: "The past is not your fault, but the future will be." Okanlami, assistant professor of family medicine, and of physical medicine and rehabilitation, said he hasn't felt any different, personally, since the protests began, because, as a Black man, this is not new territory for him. But when people ask him about it, he wants to know, "What is it that you feel? If you're coming to me with these questions, something has changed for you, which is good. Tell me what has changed, what makes this a heightened experience for you, because that's what we need to capitalize on.
"I'm trying to go beyond just reaction and emotion and move towards action."
Nearly every speaker at the Urology webinar, BMA virtual protest, and Michigan Medicine town hall expressed ideas for ways to move forward. Toward the end of the town hall, Tony Denton, J.D., M.H.A., senior vice president and chief operating officer of Michigan Medicine, presented the results of a survey that asked what the institution should do. The 1,005 responses fell into five categories, echoing many suggestions made by the speakers:
- Speak up and show solidarity through global statements, demonstrations, and zero-tolerance policies for racism.
- Create opportunities for conversations about racism in a safe space. Provide time and space to discuss those issues, and allow all voices to be heard.
- Encourage education and training. Provide educational resources on racism. Continue and bolster mandatory diversity, equity, and inclusion training for all.
- Diversify the workforce through pipelines that increase access to medical education, equitable recruitment and promotion practices, and career support.
- Work with the diverse communities that Michigan Medicine serves to address health disparities, showing that Michigan Medicine values the surrounding communities.
Runge closed the town hall by outlining some next steps. "I will ask that our Office for Health Equity and Inclusion convene a work team to do a deeper dive on the survey results and to guide us in our priorities. What we learned in the survey and other means of feedback will help this work team develop a plan around what contributions we can and must make to eliminate the racism and inequities that exist today."
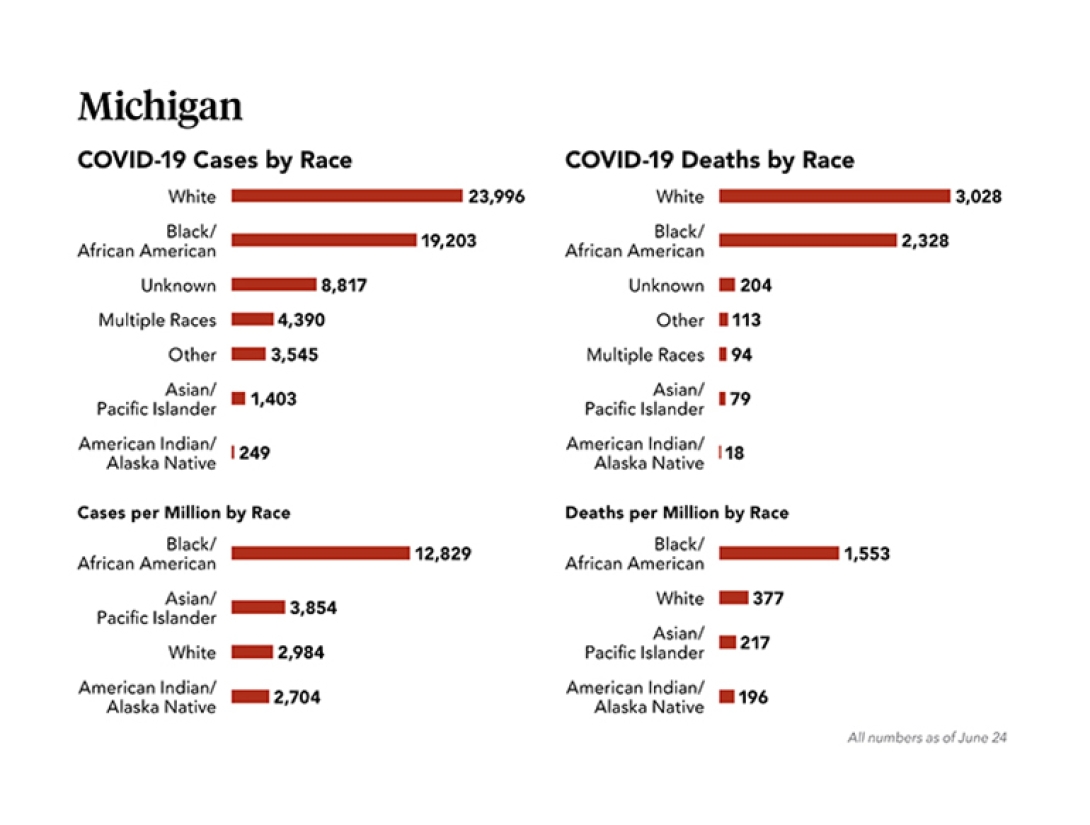
Racial Disparities in the Time of COVID-19
As the COVID-19 pandemic plays out, a startling and disproportionate death rate among Black Americans around the country is revealing persistent inequities.
"In Michigan, over 40% of COVID-19 deaths are African Americans, while only 14% of the population is made up of African Americans. This is significant, and these numbers are changing every single day," says David J. Brown, M.D. (Residency 2003), associate vice president and associate dean for health equity and inclusion at Michigan Medicine.
According to Brown, the reasons behind these unsettling findings are a complex disparity ecosystem, but this is just the latest example in a long history of systemic inequities faced by Black Americans in the U.S.
While it is true that Black Americans have higher rates of hypertension, diabetes, and obesity, all risk factors for worse outcomes from COVID-19, "I think public health practitioners would say it's not the fact that they have these diseases that's causing the higher death rate because people of all races, classes, and creeds have these diseases," says Melissa Creary, Ph.D., assistant professor of health management and policy at the U-M School of Public Health. "It's the fact that we see an undeniable burden of disease in the Black population. It's this disproportionate amount that is worrisome. The underlying issue to why we see so many is actually attributed to structural inequity."
For example, for a novel infectious disease such as COVID-19, reducing exposure is key to reducing the infection rate. This fact serves as the rationale behind stay-at-home and social distancing orders to help ease the burden on the population and the health care system. However, not everyone can stay home and still work.
"Many Black and brown people are known to have lower median incomes, which lessens the chance of an economic cushion during these uncertain times. Many can't afford to not work, or are on the front lines in jobs such as grocery clerks, janitors, or bus and train operators. Many rely on public transportation and are experiencing forced exposure," says Creary. "Economics influences these decisions. It's not about the body itself, but the societal situation in which the body is embedded."
The current "societal situation" includes not only the COVID-19 pandemic, but also the events sparked by the murder of George Floyd. The mental health impact of facing the death of family members and friends, while not being able to say goodbye or grieve together with one's community, adds to the burden of Black Americans already struggling with myriad inequities.
"Historically, groups that have been marginalized by race/ethnicity have also been oppressed by discriminatory practices which have resulted in pervasive structural and institutional practices that have further negatively affected these groups," says Adrianne Haggins, M.D. (M.S. 2012), assistant professor of emergency medicine and a member of the U-M Institute for Healthcare Policy and Innovation.
She notes that Black Americans experience a disproportionate share of environmental risk factors and are more likely to have limited economic and educational opportunities, food insecurity, and poor access to health care. "This is the persistent backdrop that has plagued communities of color, and the recent COVID-19 pandemic likely created an extraordinary stress on an already dysfunctional, ill-equipped health system serving these communities," she says.
As for theories circulated on the internet about COVID-19 disparities being due to some shared underlying genetic factor or a lack of vitamin D, Arline Geronimus, Sc.D., professor of health behavior and health education at the U-M School of Public Health, is skeptical. "It's completely implausible that there's one single factor that explains these major differences across populations."
Geronimus coined and has studied the "weathering hypothesis," which describes what happens to Black people's bodies across body systems and down to the cellular level from living in a racist society. In a racist system, the sustained high effort for Blacks of coping with environmental, psychosocial, and material stressors over years and decades and across generations leads to cellular damage and accelerated biological aging, her research shows. This results in high prevalence and early onset of chronic diseases and increased vulnerability to the worst impacts of infectious disease. She hypothesizes that weathering of the immune system could be contributing to more serious illness in these populations, even across socioeconomic lines.
"In medical school, when they teach you how to diagnose illness, they say when you hear hoof beats, think horses not zebras. Weathering is the horses and, while complex, is really right in front of our faces; there's no need to start speculating about an outsized role of vitamin D deficiency or single genes," she says.
To address this inequality, Michigan Governor Gretchen Whitmer launched an effort to study these effects via a Community Action Task Force, of which Brown is a member. "While we know that COVID-19 doesn't discriminate by race, this pandemic certainly has highlighted the racial disparities within our society, as it disproportionately impacts communities of color," says Brown. "This task force is crucial as we search for solutions for these inequities."
Michigan Medicine also assembled a Racial Disparities Advisory Committee to collect insight and experiences from health care providers within the health system. "Ultimately, it will take careful and thoughtful research disaggregated by race and ethnicity to examine the factors that drive the disparities in outcomes seen with COVID-19," says Haggins.
"Billing data and chart review may provide a glimpse into differentiating factors, but this must be coupled with hearing the voices of African American and other minority survivors and/or their family members to illuminate the experiences of these groups, in order to better understand their health care experiences and uncover the shortcomings of our health system response, and inform better outreach strategies for these vulnerable groups."
Creary hopes that efforts to understand disparities in light of COVID-19 will lead to societal changes, but notes that, historically, this hasn't been the case.
"I'm really concerned as this crisis moves into the future, when we're thinking about vaccine distribution and other areas of care and treatment, and what it might look like after we flatten the curve and are left with the aftermath. History warns us that a sustained linkage to vulnerable populations could result in eventual divestment as opposed to an investment into the lives of these populations post-pandemic."
A version of this article appeared on the U-M Health Lab Blog.





