Celebrating 10 Years of the C.S. Mott Children’s Hospital and Von Voigtlander Women’s Hospital Building
Authors |

An oral history of the building that opened in 2011 to house Mott Children's Hospital and Von Voigtlander Women's Hospital.
"Everything was on top of everything," says Edward Bove, M.D., professor of cardiac surgery and pediatrics, recalling the old C.S. Mott Children's Hospital. Patients did not have private rooms, and there was no way for parents to stay with their children. "Once a week in the old hospital, we literally used to sit down with administrators and say, 'Oh, we have to cancel [procedures] this week, because we don't have enough beds.' [Then we'd talk about how] we can't cancel this patient coming from 800 or 1,000 miles away."
At that time, there was general consensus that the old C.S. Mott Children's Hospital needed a new building, but that dream seemed like a financial fantasy. At first, the fundraising bar was $20 million. That seemed impossibly high, but Valerie Opipari, M.D., now professor of pediatrics who was chair of the department starting in 2003, believed if former patients and others understood how much a new building was needed, they would help. "People would send $5 bills, with a note: 'This is all I can do, but you saved my granddaughter's life. You saved my son's life.' The stories were incredible," Opipari recalls. "We had a grandmother who owned a bookstore in Columbus, Ohio. Every time a children's book was sold, a donation came to our building campaign."
As the campaign progressed, hospital leaders were under increased pressure to raise more funds to realize the full vision of the new building. $20 million became $50 million. Then $75 million. Each time the bar was raised, donors stepped up to meet the demand. Two major gifts — one from the Charles Stewart Mott Foundation and a naming gift for the Von Voigtlander Women's Hospital from the Ted and Jane Von Voigtlander Foundation — were instrumental in making the vision a reality. "I feel so blessed to have so many people who got behind it, so many who were willing to do the right thing for children," says Opipari.
And the right thing for women. "Our old unit was too small for our delivery volume in 2011," says Timothy R.B. Johnson, M.D. (Residency 1979), Arthur F. Thurnau Professor and professor of obstetrics and gynecology, who was chair of the department when the building opened. "Von Voigtlander Women's Hospital allowed us to provide excellent labor and delivery care and services through our family medicine, nurse midwife, and obstetrician/maternal fetal medicine practices, with our fantastic Birth Center nurses and staff, to all pregnant patients and families, including the many normal, low-risk women who seek care. On the flip side of care, VVWH allowed for the expansion of the state-of-the-art Fetal Diagnostic and Therapy Program providing fetal therapy in all the most complex and difficult categories, including reparative surgery such as myelomeningocele repair and congenital heart disease care."

"I remember when the Von Voigtlander families and their foundation gift were recognized by campaign Co-Chair Coach Lloyd Carr, and he said, 'The Von Voigtlander name will henceforth and forever be best recognized as linked to women's health at the University of Michigan.' There was not a dry eye in the house," Johnson recalls.
"One of the wisest decisions we made was keeping the C and the W [children's and women's] together and how important that is for our families," says Dee Fenner, M.D., Bates Professor of the Diseases of Women and Children and chair of the Department of Obstetrics and Gynecology. "It's really good for camaraderie, it's really good for patients. It's especially helpful for our high-risk pregnancy patients."

December 2011: Moving Day. The new C.S. Mott Children's Hospital and Von Voigtlander Women's Hospital opens. "We moved 168 patients in eight hours and four minutes. We did not have one untoward event," says Patricia Warner, MPH, former executive director of Mott and Von Voigtlander, who led much of the project to have the new building constructed. "I will tell you that when the last patient moved over to the new building, that was phenomenal."
"We had done a lot of very detailed planning. We knew that the unexpected was going to happen so we set up new operations on the fly," recalls Chris Dickinson, M.D., professor of pediatrics and chief clinical officer of Mott and Von Voigtlander. "We were moving women in labor from the women's hospital to the new Von Voigtlander Women's Hospital. We had to make decisions about who would stay and who would go. If they stayed, they were likely to deliver really soon. [We asked ourselves,] 'Do we have enough resources to resuscitate them if we need to?'
"At the end there's this sense of relief, but also exhilaration. It reminds me of when I was coaching travel hockey teams, and we would win something. You had spent all that time on preparation and everything, and even right up to the last minute, you were thinking, 'What could go wrong? Are we ready for it?' And then it is over. It's a whole wash of emotions."

"To be with your child all day and night, have your own bathroom, be in the room, was overwhelming to parents who need every little reinforcement you can give. In the old facility, they were packed three or four in a room, so they couldn't have privacy and couldn't sleep there with their baby. The new hospital was so well planned for the families," says Bove, who was named the inaugural chair of the Department of Cardiac Surgery in 2011, the year the new hospital was completed.
The decision to have private rooms "was driven by patient input," says Robert Kelch (M.D. 1967, Residency 1970), who was executive vice president for medical affairs for U-M and CEO of the U-M Health System (now Michigan Medicine) during much of the building's construction, from 2003 to 2009. "If you talk to almost any parent, when your child is under any sort of stress, you want to be there to at least share it and hopefully lessen it. You can't do that very well if you aren't in the same room. It means a hell of a lot."

"Things have changed a lot. The parents are more involved — sometimes not just emotionally, but also practically, particularly for complicated patients," says Dietrich Roloff, M.D., professor emeritus of pediatrics and communicable diseases. "I think, particularly in hematology oncology, a mother would notice something needed to be done that staff didn't pick up on. She knows her child and is often very aware of her child's treatment plan. And that kind of bedside inclusion of families is probably one of the biggest changes in patient care."
2012: 3D-printed trachea saves baby's life. Kaiba Gionfriddo becomes the first baby cured of severe tracheobronchomalacia with a 3D-printed trachea splint. The case is believed to be the first instance of a 3D-printed device saving a life. Glenn Green, M.D., professor of otolaryngology-head and neck surgery, and Scott Hollister, Ph.D., former professor of biomedical engineering and mechanical engineering and associate professor of surgery, won a Breakthrough Innovator Award from Popular Mechanics for the device. "We're talking about taking dust and using it to build body parts," says Green. "It's magical to me."

2012: Edward Bove, M.D., performs his 10,000th cardiac procedure at U-M. "I have this enormous pile of letters and pictures and, in some cases, even books that some of my patients put together as they grew up to be adults. Or their parents put together for me. It's been unbelievably heartwarming and refreshing to see them again. One letter said, 'Hi, Dr. Bove. I just graduated from college, and you operated on me when I was a 2-day-old.' You look at that, and it's pretty overwhelming."

"One of our guiding principles was, 'We will create an environment that embodies fun, optimism, humor, spirituality, and meditation.' That's what drove our concept for the environment," says Warner. "Sitting where we were, with the ability to have all of the windows looking at nature, it just made sense to incorporate the Arb." The floor of the lobby (pictured) is made partly of fossils found in Nichols Arboretum, which is adjacent to the hospital and visible from many patient rooms.
2014: First in-utero spina bifida procedure in Michigan is performed at Michigan Medicine on Carter Hilton. Carter surprised everyone when he began to walk at age 2. Since 2014, roughly 20 such procedures have been performed.

2015: Mott Family Network Pediatric Gaming Project brings Xbox consoles to patient rooms at Mott
2015: Breakthrough in Pediatric Cancer Treatment. Using a practice called precision oncology, a team of U-M researchers conducted a study that used genetic sequencing to tailor diagnoses and develop new drug treatments for cancer patients for whom standard treatments were no longer effective. Rajen Mody, M.D., professor of pediatrics and of director of the division of pediatric hematology and oncology, was the study's lead author.
2016: Denver the facility dog becomes the first full-time canine employee at Mott. Denver worked with patients in the pediatric ICU from 2016 until his retirement in 2021. Recently, generous donor support has established the Lipschutz-Danzansky Family Paws4Patients Facility Dog Program, which has four full-time service dogs working in all areas across Michigan Medicine.

2016: The Nyman Family Unit for Child and Adolescent Mental Health and Wellness opens at Mott. This is one of only a handful of children's psychiatric facilities in the state that can accept patients who may require management of co-occurring illness.
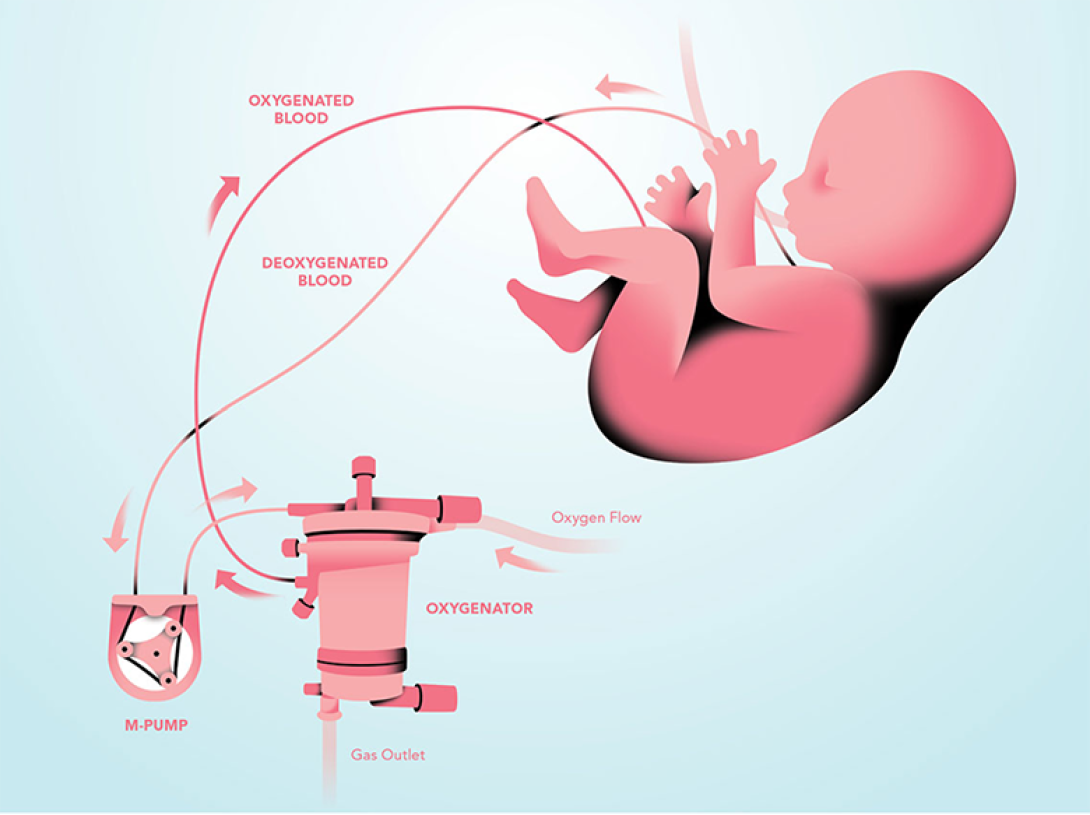
2016: Mott and U-M researchers develop an artificial placenta. The development of an artificial placenta — used successfully in premature animals — has the potential to revolutionize the treatment of extreme prematurity in infants.
2017: Ovarian Cancer Initiative is launched. The mission of the Ovarian Cancer Initiative is to fight for the lives of women with ovarian cancer through exemplary clinical care, a focus on patient quality of life, and groundbreaking research and education.
2018: Chad Carr Pediatric Brain Tumor Center is established. An incurable brain tumor took Chad Carr's life when he was just 5 years old. In 2018, a total of $30 million in gifts helped establish the Chad Carr Pediatric Brain Tumor Center. The center is designed to advance research and treatment to improve outcomes in all high-risk pediatric brain tumors.

2018: Wonder Woman joins the Mott team.

2020: Regional Infectious Containment Unit (RICU) at Mott opens to care for COVID-19 patients.

"The Department of Pediatrics was originally named the Department of Pediatrics and Communicable Diseases. The children's hospital was built on servicing children with polio and TB. That's a very rich part of our history," says Opipari, who advocated for including a negative pressure unit in the new hospital that could be used to isolate patients with highly communicable diseases. At the time, there were only two such units in the country, one on the west coast and one in Atlanta, says Opipari. The building plan was getting expensive, and some questioned whether such a unit was needed. "Who knows when the Midwest might need access to a unit you could close down, and it has its own ventilation system?" she recalls asking. She and other leaders of the building campaign were able to secure a small amount of federal funding for the RICU — the only taxpayer dollars of the entire building project — but most of the budget came from donations. "When SARS came out, we did use that unit, and we've used it since in the COVID pandemic. It was very visionary."
"Right when the pandemic started and there was so much unknown and so many executive orders coming out of the governor's office, we were just trying to keep up and advocate for children and families. I was driving into work from Royal Oak, and there were no cars on the expressway. I got to Ann Arbor, and there was no one on campus," says Luanne Thomas Ewald, MHA, chief operating officer of Mott and Von Voigtlander. "I pulled up to the hospital, and I saw that our Child and Family Life team had decorated the windows, had put positive, uplifting messages in chalk out on the sidewalk. It was very emotional. Even when there was so much uncertainty and scariness, our team came together and said, 'We need to be here for the community and for the families and kids who need us. We're going to try to bring calm, peace, and motivation to families, kids, and to each other.' It was a small gesture that had a huge impact."
2020: Conjoined twins separated at U-M. "The day that we operated on the conjoined twins highlighted the strength of services within the building, which was uniquely designed to have the women's hospital and children's hospital in the same building," says Ewald. "After another facility could not help this family, they sought our Maternal Fetal Medicine team, even before the babies were born. We were able to help them at Michigan Medicine. The family had complete confidence in our team and became familiar with the team here, the building here, and the babies were delivered here."
"You see the video of the surgeon saying, 'They're separated,' and it was really emotional for me," says Ewald. "That is really what the building and the team were designed for, to do this high-level care and to have all of the teams involved. It was literally everyone from valet to housekeeping to security, in addition to the care team, who became part of this family's family."
"What has worked better than I could have anticipated is having a women's hospital on the same unit and building as the children's hospital," says Dickinson. "We can do all sorts of unusual operations, procedures, and treatments, for the mom and baby, all under one roof and bring large numbers of specialists together in order to make it all happen."

"How would you count all the lives that have been saved in Mott Hospital? I'd love to be able to gather all those children together and look at them. It would be a very impressive picture," says Donna Martin (M.D. 1996, Ph.D. 1992, Residency 1999, Fellowship 2001), chair of the Department of Pediatrics, the Ravitz Foundation Endowed Professor of Pediatrics and Communicable Diseases, and professor of human genetics.